Result Area #1: Improved Quality of Care
Recognizing that there is no single silver bullet in quality of care, the Program embraces a multipronged approach to quality improvement. It is built around the same key universal actions for improving quality of care as outlined in the Lancet Global Health Commission on High Quality Health Systems in the SDG Era:17 (a) govern for quality, (b) transform the health workforce through competencybased clinical education, and (c) ignite the demand for quality in the population and improve accountability. The Program addresses each pillar through various quality improvement interventions as illustrated in the below figure. These interventions are aligned with best global practices, and the focus on clinical processes rather than structural interventions is supported by global evidence
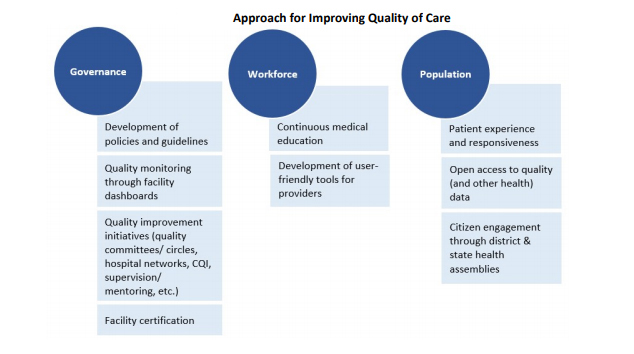
First, the Program will improve governance through the development of clinical protocols/guidelines; monitoring quality of care using facility dashboards; introducing and scaling up clinical governance and other quality improvement initiatives (quality committees, hospital quality networks, continuous quality improvement, and strengthened supervision/mentoring); and facility certification. With respect to certification, the Program supports national accreditation for 370 primary-, secondary-, and tertiary-level health facilities in the public sector. Two types of certification will be sought: National Quality Assurance Standards (NQAS) for primary- and secondary-level facilities and National Accreditation Board for Hospitals and Healthcare Providers (NABH) for tertiary-level facilities (medical colleges). The former has been used in the public sector in India while the the latter has been used in the private sector. Tamil Nadu currently has three public secondary hospitals certified with NQAS or NABH and four primary health centers (PHCs) and community health centers (CHCs) certified with NQAS. This set of quality improvement measures will improve accountability by strengthening the feedback loops within health facilities as well as between health facilities and the state.
Second, expansion of the continuous medical education (CME) program and development of userfriendly decision support tools for providers will strengthen the workforce. CME will be expanded to include not only physicians but also nurses and paramedics. These interventions together will strengthen both clinical quality of care at a provider level as well as the state’s regulatory role.
Finally, the Program will engage the population through the development and introduction of patient experience questionnaires, making quality and other data accessible to the public, and conducting district and state health assemblies. The quality dashboard and patient experience survey will ignite the demand for quality in the population and improve accountability by strengthening the feedback loops between citizens and facilities as well as between facilities and the state. The health assemblies will strengthen the feedback loop between citizens and the state.
Two disbursement-linked indicators (DLIs) directly support this result area. DLI #1 is a scaleable indicator with an allocation of US$43.7 million and DLI #2 is a scaleable indicator with an allocation of US$38.2 million. DLI #1 supports institutional reforms to support quality improvement including the development and adoption of a Quality of Care (QoC) Strategy, development and rollout of the quality dashboard, and other quality improvement initiatives. DLI #2 supports the accreditation of public facilities. DLI #2 is also a prior result, with the expectation that 11 primary- and 34 secondary-level facilities will receive NQAS certification before signing of the loan. In addition, other DLIs that are cross-cutting in nature and described at the end of this section also support improvements in quality of care (DLIs #6, #7, and #8).
Result Area #2: Strengthened Management of Non-Communicable Diseases and Injuries
The second result area focuses on enhancing the management of NCDs, associated risk factors and injuries. NCD interventions under the Program represent the continuation and further scaling-up of the successful Tamil Nadu NCD initiatives previously supported by the World Bank, mainstreamed into Tamil Nadu’s health sector activities, and fed into the National Program for Prevention and Control of Cancers, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). Tracer conditions for NCD response supported by the Program include hypertension, diabetes, cervical cancer, breast cancer, oral cancer, and mental health. NCD interventions under the Program focus on the following areas: (a) health promotion and NCD prevention, (b) population-based screening of NCDs among the eligible population, (c) treatment and follow-up, and (d) improvement of monitoring and evaluation related to NCDs. To improve health promotion and NCD prevention, a comprehensive social and behavior change communication (SBCC) strategy will be developed that includes multiple layers of engagement with patients, health providers, and communities through various channels of communication. As part of the SBCC strategy, patient empowerment mechanisms will be established to transform patients, especially those with chronic conditions, from being passive recipients of care into proactive participants who are equipped with knowledge and skills for self-management of their conditions.
To improve coverage of screening for NCDs, the Program will support the implementation of population-based screening for which new guidelines have been issued. Under the new guidelines, field functionaries (Accredited Social Health Activist, Women Health Volunteers, and Anganwadi Workers) are expected to make house visits, raise awareness of NCDs and risk factors, screen for hypertension and diabetes, and refer to a PHC for further follow-up. This population-based screening approach will be integrated with the establishment of health and wellness centers (HWCs) and strengthening of PHCs at the lowest level to improve treatment and follow-up for patients diagnosed with NCDs. In addition, the Program will contribute to strengthening lab services and improving health provider capacity to address mental health. To improve monitoring and evaluation related to NCDs, the Program will include the development of NCD care cascades for selected tracer conditions (for example, hypertension and diabetes), as well as strengthening of data on NCDs and mental health for better planning and management. While the Program will focus on NCD response within the health sector, the comprehensive NCD response will require a multisectoral approach. To facilitate this approach, a multisectoral coordination mechanism will be established to support the state’s NCD response. Many of the quality of care interventions discussed under Result Area #1 will also benefit NCD management.
Given the high prevalence of road traffic accidents and other injuries, the Program scope will include addressing injuries. Tamil Nadu has an advanced Emergency Medical Services (EMS) work plan which adequately covers both pre-hospital and in-hospital EMS. The Program will support the implementation of the EMS work plan, including emphasis on further strengthening the 108 ambulance services to improve pre-hospital care, including improvements in IFT protocols and expansion of the 108 ambulance fleet. The Program will also improve in-hospital care by strengthening the provision of 24x7 trauma care services at Level 1 and Level 2 emergency departments and establishment of a trauma registry. Under the Program, as part of the Tamil Nadu Accident and Emergency Care Initiative (TAEI) initiative, Level 3 and Level 4 training will be provided to emergency department trauma care providers and other health care workers to strengthen both pre-hospital and in-hospital care.
The following two DLIs directly support this result area. DLI #3 is a scaleable indicator with an allocation of US$48.9 million, and DLI #4 is a scaleable indicator with an allocation of US$17.7 million. DLI #3 on diabetes and hypertension under control reflect efforts in prevention, screening, treatment and follow up (including patient tracking) of NCDs and their associated risk factors. DLI #4, which addresses the management of injuries, includes intermediate results in both pre-hospital care (improved IFT in the 108 ambulance service) and in-hospital care (the establishment of trauma registries and strengthening provision of services in trauma centers). Cross-cutting DLIs #6, #7 and #8 also support improvements in management of NCDs and injuries.
Result Area #3: Reduced Equity Gaps in Reproductive and Child Health
A special focus will be maintained in nine priority districts, which constitute the bottom quintile of the RCH indicators in the state and have a relatively large proportion of tribal populations. The six priority districts based on poor performance on RCH indicators are Ariyalur, Ramanathapuram, Theni, Thoothukkudi, Tirunelveli, and Virudhunagar. Three indicators have been chosen to assess progress in this domain: full immunization, full ANC, and modern contraceptive prevalence rate. The three additional districts with relatively large ST populations are Dharmapuri, The Nilgris, and Tiruvannamalai.
Interventions in the Program to reduce inequities between districts focus on a combination of supply- and demand-side interventions to support increased utilization of RCH services. The state provides mobile outreach services for tribal populations through 20 mobile medical units operated by nongovernmental organizations (NGOs) in tribal blocks. The mobile outreach team offers minor ailment treatment, antenatal screening, NCD screening, and lab tests. Drugs are also provided free of charge. Additional supply-side interventions that will be introduced through the Program include better provision of quality RCH services as indicated by NQAS certification of primary and secondary care facilities. Furthermore, maternity stay wards will be established in remote areas to facilitate continuum of care before, during and after delivery which will positively impact both immunizations and contraceptive uptake. Other quality of care interventions under Result Area #1 will also benefit the provision of RCH services. Demand-side interventions include the development and implementation of the SBCC strategy tailored to these priority districts. A household RCH survey will be administered in the priority districts to not only track progress on the service coverage indicators (and DLIs) but also better assess demand-side barriers over time which will also facilitate course corrections in implementation as needed.
The following DLI directly supports this result area. DLI #5 is a scaleable indicator with an allocation of US$56.5 million. It supports and tracks the utilization of three RCH services in the priority districts. They are (a) full immunization of children under age 2, (b) full ANC for pregnant women, and (c) modern contraceptive prevalence rate among women of reproductive age. In addition, DLI #2 on certification of public health facilities also supports this result area through higher payments for certification of facilities in the priority districts. Finally, the cross-cutting DLIs (#6, #7, and #8) also support results on equity in RCH services.
Cross-Cutting Initiatives to Strengthen Institutional and State Capacity to Achieve the Above Results
The Program also supports cross-cutting initiatives to strengthen institutional and state capacity to achieve the above three result areas. These interventions aim to improve ‘how’ the sector operates and complement the technical interventions discussed above in the three result areas (‘what’ specifically the sector does). As such, these interventions fall along the causal chain of results on quality of care, NCDs and injuries management, and RCH equity. Good practices and innovations from Tamil Nadu are being scaled up while others from around the world are being introduced through the Program to improve management of the public health sector, increase transparency, and strengthen accountability. These key ‘hows’ will enable Tamil Nadu to move from a focus on access to an increasing focus on quality of care. These systematic reforms will also better position the state to tackle emerging disease patterns that require a different approach to service delivery while simultaneously closing the remaining gaps on last mile delivery of basic RCH services. Finally, the PforR instrument—with a focus on achievement of outputs and outcomes—will help the sector realign planning, budgeting, expenditures, and coordination to defragment implementation and ensure the achievement of results. With this innovative and forwardlooking approach, Tamil Nadu will offer lessons and set the stage for other states to follow suit. Box 1 below provides details about these initiatives and how they will enhance public health sector management.
The following three DLIs directly support this cross-cutting agenda: DLI #6 is a scaleable indicator with an allocation of US$36.5 million, DLI #7 is a scaleable indicator with an allocation of US$30.75 million, and DLI #8 is a non-scaleable indicator with an allocation of US$14 million. DLI #6 aims to stimulate strengthening the content, quality, accessibility, and use of the health information system for decision making. DLI #7 is about building state capacity to improve planning and implementation, including performance-based management. DLI #8 supports transparency, collaborative social accountability, and consolidation of citizen engagement through annual district and state health assemblies. This will further strengthen the feedback loops between citizens and the state.
The theory of change for the Program is illustrated in Figure 4, starting with challenges identified and followed by the inputs, expected outputs and intermediate results, and expected outcomes. As indicated, a subset of intermediate results and expected outcomes have been selected as DLIs.